Acute pancreatitis: If your doctor suspects that you have acute pancreatitis, a sample of your blood may be analyzed for abnormalities such as:
- Elevated levels of the pancreatic enzymes, amylase and lipase;
- Elevated white blood cell count;
- Elevated liver enzymes and bilirubin, a substance that results from breakdown of red blood cells;
- High blood sugar (hyperglycemia);
- Low calcium level — high calcium levels can cause pancreatitis, but low levels of calcium in the blood, called hypocalcemia, are a common result;
- Blood tests. These tests can identify abnormalities associated with chronic pancreatitis and help rule out acute inflammation.
- Stool test. This measures the fat content in your feces. Chronic pancreatitis often causes excess fat in your stool because the fat isn't digested and absorbed normally by your small intestine.
- Ultrasound. In standard (external) ultrasound, a wand-like device (transducer) is placed on your body. It emits inaudible sound waves that are reflected to the transducer and then translated into a moving image by a computer. Endoscopic ultrasound may provide images of your pancreas and bile and pancreatic ducts that are superior to those produced by standard ultrasound.
- EUS. In endoscopic ultrasound, your doctor uses a thin, flexible tube with a light (endoscope) to thread a small ultrasound device through your stomach. The device then generates a detailed image on a computer screen.
- ERCP. X-ray of bile and pancreatic ducts. In a procedure called endoscopic retrograde cholangiopancreatography, your doctor gently threads an endoscope down your throat and through your stomach to the opening of the bile and pancreatic ducts in your duodenum. A dye passed through a thin, flexible tube (catheter) inside the endoscope allows for X-ray images of the ducts.
Fig. 1. Pancreas with no dialation of Main Pancreatic Duct and no clubbing of side branches.
....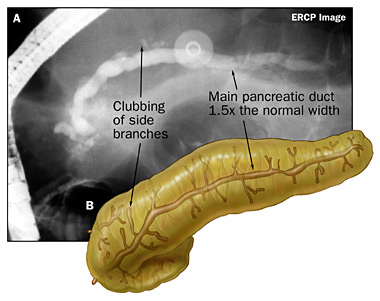
Fig. 2. Pancreas with main pancreatic duct dialated to 1.5x normal width and some clubbing of side branches.
Fig. 3. Pancreas with main pancreatic duct dialated to > 1.5x normal width and clubbing of side branches.
...
- Pancreatic function test. If you've lost weight or your doctor suspects a malabsorption problem, you may have a pancreatic function test. Several tests exist, but all measure the ability of your pancreas to secrete enzymes or other substances necessary for digestion.
- SSMRC. MRCP With Secretion Stimulation. IV injection of synthetic secretin, a gut hormone, causes a rapid outpouring of bicarbonate-rich fluid from the exocrine pancreas. SSMRCP provides significantly improved visualization not only of the main PD, but also of its side branches, when compared to nonstimulated imaging.
- You may need additional tests if your doctor is concerned about the possibility of other diseases, such as pancreatic cancer. Chronic pancreatitis puts you at a slightly higher risk of pancreatic cancer.
- Infection. A damaged pancreas may become infected with bacteria that spread from the small intestine into the pancreas. Signs of infection include fever, an elevated white blood cell count and, in severe cases, organ failure. A fluid sample from the pancreas may be tested for bacterial infection. Pancreatic infections can be fatal without intensive treatment, including drainage or surgery to remove the infected tissue. Sometimes multiple operations are necessary.
- Pseudocysts. These are collections of pancreatic fluid and sometimes tissue debris that form within the pancreas or in an obstructed duct. If the cyst is small, no special care may be necessary, but large, infected or bleeding pseudocysts require immediate treatment.
- Abscess. This is a collection of pus in or near your pancreas that may develop about four to six weeks after the onset of acute pancreatitis. Treatment involves drainage of the abscess by catheter or surgery.
- Respiratory failure. Chemical changes in your body can affect your lung function, causing the level of oxygen in your blood to fall to dangerously low levels.
- Shock. This life-threatening complication usually occurs when your blood pressure is so low your organs can't carry out their normal functions. Severe shock can cause death within minutes if left untreated.
- Bleeding. Ongoing inflammation and damage to the blood vessels surrounding the pancreas can cause potentially fatal bleeding.
- Malnutrition and weight loss. Lack of digestive enzymes prevents your body from absorbing nutrients from food. The result is often unintended weight loss and malnutrition.
- Diabetes. Damage to insulin-producing cells can lead to diabetes, a disease that affects the way your body uses blood sugar.
- Drug dependency. Because medical treatments for severe pancreatic pain aren't always effective, people with pancreatitis may become dependent on pain medications.
- Pancreatic cancer. Long-term inflammation of the pancreas increases your risk of pancreatic cancer, one of the most serious of all malignancies.
..
Why Pain?
The role of mast cells in the pathogenesis of pain in chronic pancreatitis.
BMC Gastroenterol. 2005; 5:8 (ISSN: 1471-230X)
Hoogerwerf WA; Gondesen K; Xiao SY; Winston JH; Willis WD; Pasricha PJEnteric Neuromuscular Disorders and Pain Laboratory, Division of Gastroenterology and Hepatology, University of Texas Medical Branch, 301 University Boulevard, Galveston, TX 77555-0764, USA. wahooger@utmb.edu
- BACKGROUND: The biological basis of pain in chronic pancreatitis is poorly understood. Mast cells have been implicated in the pathogenesis of pain in other conditions. We hypothesized that mast cells play a role in the pain of chronic pancreatitis.We examined the association of pain with mast cells in autopsy specimens of patients with painful chronic pancreatitis. We explored our hypothesis further using an experimental model of trinitrobenzene sulfonic acid (TNBS) -induced chronic pancreatitis in both wild type (WT) and mast cell deficient mice (MCDM).
- METHODS: Archival tissues with histological diagnoses of chronic pancreatitis were identified and clinical records reviewed for presence or absence of reported pain in humans. Mast cells were counted.The presence of pain was assessed using von Frey Filaments (VFF) to measure abdominal withdrawal responses in both WT and MCDM mice with and without chronic pancreatitis.
- RESULTS: Humans with painful chronic pancreatitis demonstrated a 3.5-fold increase in pancreatic mast cells as compared with those with painless chronic pancreatitis. WT mice with chronic pancreatitis were significantly more sensitive as assessed by VFF pain testing of the abdomen when compared with MCDM.
- CONCLUSION: Humans with painful chronic pancreatitis have an increased number of pancreatic mast cells as compared with those with painless chronic pancreatitis. MCDM are less sensitive to mechanical stimulation of the abdomen after induction of chronic pancreatitis as compared with WT. Mast cells may play an important role in the pathogenesis of pain in chronic pancreatitis.
To view information on another disease, click on Pancreatitis SOD Library.!
..


No comments:
Post a Comment